SIRT (Selective Internal Radiation Therapy)
Treatment for Liver Tumors & Stage IV Colorectal Cancer
When you or a loved one has been diagnosed with a liver tumor, or stage IV colorectal cancer, it is important to learn the facts and evaluate treatment options. Whether your cancer originated primarily in the liver, or has spread from the colon to the liver, you may be a candidate for liver-directed radiation therapy or other liver-directed therapies provided at Methodist Dallas Medical Center.
Generally colorectal cancer stage IV means the cancer has spread to distant locations in the body (metastasized). The primary site of metastasis for colorectal cancer is the liver. Of the nearly 140,000 Americans diagnosed with colorectal cancer every year, at least 60 percent will see their cancer spread to the liver. While most liver tumors are surgically inoperable, Selective Internal Radiation Therapy (SIRT) or other local therapies may provide a practical way to treat inoperable liver tumors that have metastasized from the colon.
What Is Selective Internal Radiation Therapy?
SIRT (Selective Internal Radiation Therapy) is a form of liver-directed therapy that uses the liver’s unique blood supply to deliver and implant millions of yittrium-90 (Y-90) microspheres to directly target the arterial supply of the tumor. Here the radioactive microspheres become trapped, killing tumor cells and mostly sparing the surrounding healthy liver tissue. Most therapeutic radiation is delivered in 11 days, with minimal radiation remaining after one month.
How Is The Treatment Performed & Will I Need To Stay In The Hospital?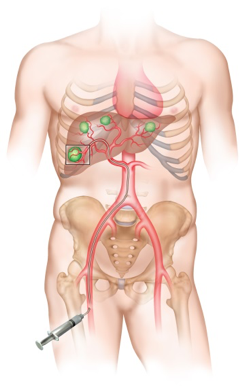
An interventional radiologist performs the Y-90 radioembolization procedure. A microcatheter is threaded through a femoral artery puncture into the hepatic artery that supplies the liver tumors. Millions of microspheres are delivered directly to the tumor, and become trapped in the microvascular tumor bed and emit beta radiation to the tumor. This allows the surrounding healthy liver to remain unaffected, which maximizes effectiveness and allows the patient to have a good quality of life. The treatment is typically administered as an outpatient procedure, minimizing the time spent at the hospital. Patients are typically released within three hours after the treatment.
Is The Treatment Safe & Effective?
Clinical studies have shown SIRT with microspheres slows disease progression and increases overall survival without adversely affecting the patient’s quality of life. In clinical studies, microspheres have been combined with modern chemotherapy or administered as a single therapy during a break from chemotherapy. SIRT has been proven to decrease tumor burden in the liver, increase time-to-disease progression and survival time, potentially downsize tumors in the liver to allow surgery (resection or ablation), and provide relief from symptoms.
Treatment with Y-90 resin microspheres is recommended by the National Comprehensive Cancer Network (NCCN). NCCN is an alliance of 27 of the world’s leading cancer centers that work together to develop treatment guidelines for most cancers. The NCCN panel includes Y-90 microspheres as a Category 2A treatment recommendation in its Clinical Practice Guidelines for colon cancer and rectal cancer. These guidelines set standards for best practice, and assist patients and providers in the decision-making process for cancer treatment.
How Will I Feel After Treatment?
Almost all treatments and drugs produce potentially unwanted side effects. Most side effects following a SIRT procedures are minor and do not last long, but a small number can be serious. Every patient is different in how he or she reacts to a treatment. In the first few weeks after the procedure many patients experience abdominal pain and/or nausea. This typically subsides after a short time and can be managed with medications. Patients may also develop a mild fever and feel more tired than usual, which may last for several weeks. In rare instances a small number of microspheres may inadvertently reach other organs in the body, such as the stomach, intestine or pancreas. These complications are rare, but if they do occur they may require additional medical treatment.
Contact Us at 214-933-6601 for more information or to schedule an appointment
Y-90 ADVANCED TREATMENT CENTER at Methodist Dallas Medical Center
 Experienced Providers
Experienced Providers
A diagnosis of liver tumors can be overwhelming. As with any highly technical, specialized care, patients should seek a high-volume treatment center for their care. Methodist Dallas operates one of the most well established Y-90 Advanced Treatment Centers in Texas with a proven track record for safety and positive outcomes. With a high success rate for liver transplants in the Dallas area, Methodist Dallas Medical Center has earned a respected reputation for liver care.
Multidisciplinary Team Approach
Our multidisciplinary team of experts offers hope and personalized care to patients and their families with this diagnosis. Our team believes each patient is unique, and collaborates across disciplines to provide personalized treatment recommendations for each case. Each case is reviewed by the treatment team consisting of oncologists, surgeons, interventional radiologists, and others. A dedicated nurse navigator facilitates and coordinates your care to ensure clear communication with you and your providers, consistency in care between providers, and timeliness of the services you receive.
Methodist Dallas Provider Team
Islam A. Shahin, MD
Interventional Radiologist
Medical Director, Interventional Radiology, Methodist Dallas Medical Center
Parvez Mantry, MD
Hepatologist, Gastroenterologist
Medical Director, Liver Institute Research
Medical Director, Hepatobiliary Tumor Program
Associate Program Director for the Fellowship in Gastroenterology and Hepatology,
Methodist Dallas Medical Center
Alejandro Mejia, MD, FACS
Hepatobiliary-Transplant Surgeon
Executive Program Director, Organ Transplant
Vichin Puri, MD, FACS
Hepatobiliary - Transplant Surgeon
Atisha P. Manhas, MD
Hematologist and Medical Oncologist
Principal Investigator, US Oncology Research
 Nurse Navigator Services
Nurse Navigator Services
An oncology trained registered nurse called a Nurse Navigator serves as your personal guide. She is well versed in cancer treatment and is well acquainted with the healthcare system and how it operates. She works with you and your providers throughout the process to ensure your understanding of the recommendations and the course of treatment, as well as helps you overcome any road blocks you may encounter along the way. Her knowledge and experience helps ease your passage throughout your journey. The nurse navigator is available to patients on an inpatient and outpatient basis to:
- Answer questions and assist you in getting information
- Ease access to appointments and help you get services you need in a timely manner
- Clarify and reinforce patient education
- Facilitate collaboration between healthcare providers to develop treatment plans for Y-90 treatment
- Coordinate office visits across medical disciplines to streamline your care
- Support communication between you and all members of the healthcare team
- Smooth transition to ongoing care in your community
- Link you with additional support services and resources in your community to ensure continuity of care
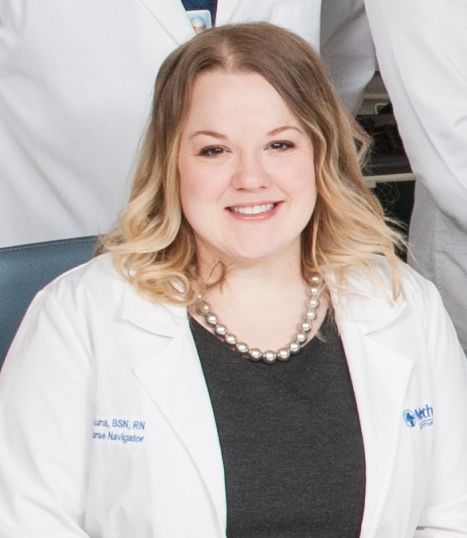 Candice DeLuna, BSN, RN
Candice DeLuna, BSN, RN
Nurse Navigator
Candice DeLuna graduated with honors from the El Centro College nursing program in 2012. She went on to earn her Bachelor of Science degree in nursing from the University of Texas at Arlington. As an Oncology Nurse Navigator, Candice works closely with patients and their families to help them find and obtain the treatment they need. On a daily basis she exhibits a passion for keeping the patient informed and ensuring that the patient’s best interest is at the center of treatment planning. She applies a three-step approach to every patient encounter – 1. Educate 2. Empower 3. Advocate.
Contact Us at 214-933-6601 for more information or to schedule an appointment
Patient Resources
Cancer Support Group
General Cancer Support Group Meeting
When: Fourth Monday of every month
Time: 6 to 7:30 p.m. (Refreshments are provided)
Location: Methodist Dallas Medical Center
1441 N. Beckley Ave., Dallas, TX 75203
7 Schenkel Bed Tower-Hitt Family Room
Contact: Michelle Muir at 214-947-7099 for more information.
Cancer Support Group Meeting en Español
When: Second Thursday of every month
Time: 6 to 8 p.m. (Dinner provided)
Location: Methodist Dallas Medical Center
1441 N. Beckley Ave., Dallas, TX 75203
Weiss Auditorium–Weiss Building
Contact: Eva Hernandez at 214-947-2924 for more information.
 Beat Liver Tumors
Beat Liver Tumors
YES, You Can Too is a group of patients, families, and caregivers who understand what you’re experiencing and want to help. Our growing international network is here to provide a variety of support services to patients and families just like you – whether you need advice, guidance, or just someone to lend a listening ear. In addition, YES members advocate for increased funding for cancer research and education for liver tumor survivors about possible surveillance and treatment options.
Founded by three stage 4 colon cancer survivors and two cancer caregivers in October 2006, YES embraces the motto, "When the Improbable is Possible.” Members participate by sharing resources and information online, attending teleconferences, lobbying federal and state legislators and speaking at conferences and health fairs. More recently, YES began an awareness campaign targeted at the medical community to encourage doctors and researchers to focus more resources on patients just like you.