Complications of Cirrhosis
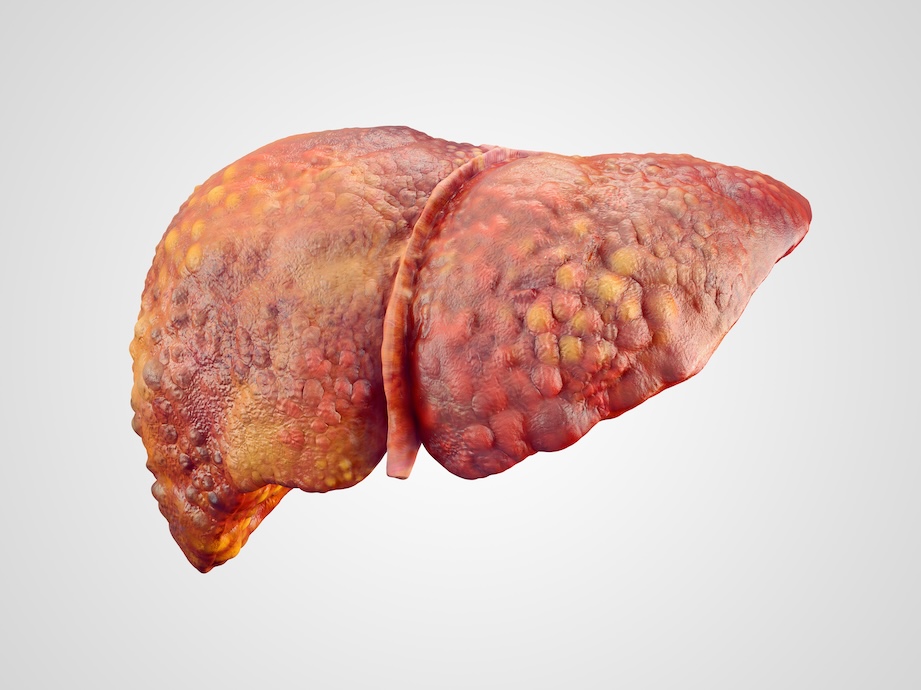
Cirrhosis is defined as severe scarring of the liver and is caused by a number of liver diseases and conditions. Patients with cirrhosis, may experience complications of this condition. Below we discuss the most common complications of cirrhosis.
Ascites
Ascites is the most common complication of cirrhosis. It happens when fluid builds up in the abdomen, causing the belly to swell.
How does this happen? Cirrhosis damages the liver and slows blood flow through it. This can raise pressure in the portal vein, a condition called portal hypertension. As a result, your kidneys may retain too much salt and water. Over time, this extra fluid can accumulate in your belly.
The main symptoms of ascites include a swollen belly and rapid weight gain (for example, two or three pounds per day over several days). Some people may also notice swelling in the ankles (edema), shortness of breath, trouble moving, digestive problems, fatigue, and back pain.
Ascites is treated using paracentesis, a medical procedure that involves removing excess fluid from the abdominal cavity. Paracentesis relieves pressure on abdominal organs, helps improve breathing, reduces pain and discomfort.
Portal hypertension
Portal hypertension is a condition where the pressure in the portal vein—the large vein that carries blood from the digestive organs to the liver—is higher than normal. It most often occurs in people with cirrhosis, a disease that causes scarring of the liver. When the liver becomes stiff from scarring, blood flow through it slows down, causing pressure to build up in the portal vein.
Hepatic encephalopathy (HE)
A serious condition that occurs when the liver is not able to properly filter toxins from the blood, this includes filtering ammonia from the intestines.
When the toxins buildup, it affects the brain's ability to function normally. If left untreated or unsuccessfully treated, patients can experience severe neurological symptoms such as unresponsiveness, coma or death.
Estimates say that about 30% to 40% of people with cirrhosis experience HE. There are three types of HE, with Type C being the type that occurs due to cirrhosis.
Symptoms to watch for:
- Trouble with focus & concentration
- Disorientation or confusion
- Slurred speech
- Personality/mood changes
- Memory loss
- Daytime fatigue, nighttime wakefulness
- Flapping tremors in arms/legs
- Coma
If you or someone with liver disease experiences sudden confusion, unusual behavior, or cannot be awakened, contact a healthcare professional or go to the emergency room immediately.
Hepatorenal Syndrome (HRS)
Hepatorenal syndrome (HRS) is a serious, life-threatening complication of advanced liver disease. It usually occurs in people with chronic, progressive liver disease who are approaching liver failure.
HRS can lead to kidney failure in people with or without prior kidney problems. If HRS develops, urgent medical attention is required, and in most cases, a liver transplant is the only effective treatment.
In hepatorenal syndrome, liver failure causes the blood vessels in your kidneys to narrow, reducing blood flow. As a result, your kidneys stop working properly because they don’t receive enough blood.
The most common factor identified as the cause of HRS is portal hypertension.
spontaneous bacterial peritonitis
Spontaneous bacterial peritonitis is an infection of the fluid accumulated in the abdomen (called ascites). This infection can occur when bacteria that normally live in the intestine enter the abdominal cavity and the ascites becomes infected.
Typically seen in end-stage liver disease when the immune system is compromised and the gut environment has changed, the biggest risk of this condition is sepsis. Sepsis is a rapid spread of infection throughout the body.
Your hepatologist can take a small sample of the ascitic fluid, using a small needle & syringe, to test for spontaneous bacterial peritonitis. If diagnosed with this condition, treatment consists of IV antibiotics.
Jaundice
Jaundice occurs when a damaged liver cannot remove enough bilirubin, a waste product, from the blood. This leads to yellowing of the skin and the whites of the eyes, as well as dark-colored urine. Symptoms may also include fatigue, abdominal pain, and nausea.
Treatment focuses on addressing the underlying cause, and early medical evaluation is important to prevent complications.