Kidney Pre-Transplant Surgery
Guide
Kidney and Pancreas Pre-Transplant Surgery Guide
Important Phone Numbers
Methodist Dallas Medical Center |
214‐947‐8181
Kidney and Pancreas Transplant Program |
214‐947‐1800
Dallas Nephrology Associates |
214‐358‐2300
- Dr. Jose Castillo‐ Lugo
- Dr. Kosunarty Fa
- Dr. Muhammad Qureshi
- Dr. Ruben Velez
- Dr. Wael Hanna
Dallas Renal Group | 972‐274‐5555
- Dr. Amna Ilahe
- Dr. Silvi Simon
Texas Urology Specialists | 214‐948‐3101
- Dr. Sujeet Acharya
- Dr. Jeffrey Toubin
About the Kidney
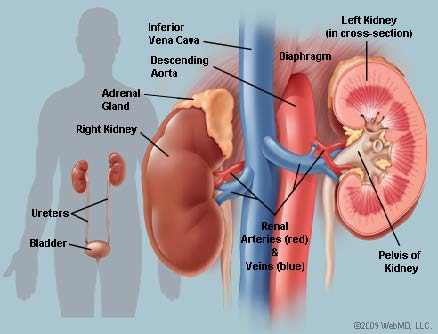
Anatomy
The kidneys are bean‐shaped organs that remove waste products and salts from the
blood and empty them in the urine. They are in the back of the abdomen,
behind the
intestines and under the ribs at about the level of the waistline. One
kidney lies
on either side of the spine. Each weighs about a third to half a pound
and has a duct
(called a ureter) on its inner surface. The ureter, in adults it is about 10 to 11
inches long, carries urine from the kidney to the bladder, where the urine
is temporarily
stored. Another duct (called the urethra) carries the urine from the bladder
to outside the body.
Functions
The main function of the kidneys is to make urine and maintain the normal makeup of
the blood. Kidney functions include:
- Reabsorb water to maintain water balance
- Filter and reabsorb sugars, protein, sodium, and chloride that are useful to the body
- Filter and remove (by means of urine) things that are not useful to the body, such as urea, uric acids, and creatinine
- Make and remove ammonia to help keep the body’s acid‐base balance
- Produce hormones that stimulate red blood cell production and regulate blood pressure.
Transplanted Kidney
While hemodialysis or peritoneal dialysis can eliminate waste and excess
chemicals from
your blood, unlike the kidneys it cannot produce vital hormones. Through
transplantation, you will receive a new kidney that performs all of these important
functions, and you won’t have to continually interrupt your life
for dialysis treatments or
depend on machines to keep you going. Whether your kidney is from a living donor or
from a deceased organ donor, it will truly be a gift of life.
The transplanted kidney will be placed in your lower abdomen. This placement is
preferred because your own (or “native”) kidneys are not removed
unless they are
causing you problems and it is easier to biopsy the new kidney in this position.

Methodist Dallas Medical Center Informed Consent for Kidney and Pancreas Transplant Patients
Evaluation Process
You will be evaluated with consultations, lab tests, and various procedures
to determine
the appropriateness of transplant. You will meet with many members of the
transplant
team who may include:
- The Transplant Coordinator provides education regarding the transplant evaluation process, listing for transplant, and patient responsibilities before and after transplant. This meeting is intended to provide you with an opportunity to ask questions and to become fully informed about the transplant process.
- A Transplant Nephrologist is a physician who specializes in kidney disease. The Transplant Nephrologist assesses medical suitability for transplantation, discusses the significance of transplantation (including alternatives and potential medical complications), manages transplant‐related medical needs before and after transplant, participates in care during the transplant hospital admission, and follows transplant recipients during clinic appointments at specific time periods post‐discharge.
- A Transplant Surgeon will meet with you during the evaluation and/or prior to surgery to discuss the appropriateness of a transplant based on the information obtained during your evaluation. The Transplant Surgeon evaluates surgical suitability for transplant, discusses the significance of transplantation with the patient (including the risks, benefits, and surgical complications), discusses the various types of organs available, performs the operation, and provides postoperative care for a defined period of time following surgery.
- An Anesthesiologist may meet with you and review your medical records to determine the need for any additional workup to determine your risk from anesthesia.
- A Social Worker will meet with you to evaluate your ability to cope with the stress of transplantation and your ability to follow a rigorous treatment plan, both before and after transplantation. The social worker will also help to identify your support network. They will discuss psychological risks, the costs associated with your transplant, and the costs associated with the medications you will require after transplant. They will also work with you to help you understand your insurance coverage. It is important that you understand the costs that may not be covered by insurance.
- A Psychiatrist/Psychologist may conduct a more in‐depth evaluation and assessment. Some patients with a history of drug or alcohol abuse may be required to participate in a rehabilitation program and meet abstinence requirements prior to and after transplant listing.
- A Registered Dietitian will perform a nutritional assessment and provide nutrition education.
-
Some patients may be referred to another service for consultation. For example,
many patients need to be seen by a pulmonologist (lung doctor) or a cardiologist
(heart doctor) to assess for other medical conditions.
Many different tests are done to determine if you are a suitable transplant
recipient.
Some of the following tests may be included in your evaluation process. Remember,
other tests may need to be done based on the results of these tests.
-
Blood tests help to determine the extent and/or cause of your kidney and/or
pancreas disease. Other tests will determine your blood type for organ matching
and screen for your immunity to or the presence of specific viruses, including
HIV. Additional blood tests may be used to determine how well other organs are
functioning. - A chest x‐ray helps your physician identify any problems with your lungs
-
An EKG, echocardiogram and/or stress test will show how well your heart is
beating and the function of your heart valves. This will help your physicians
decide if your heart function is strong enough for transplant surgery. -
An ultrasound of your kidneys and abdomen helps assess the size, shape, and
circulation of your kidneys and/or pancreas. -
Pulmonary function tests may be required, especially if you have a history of
smoking or a history of lung disease. This is a breathing test to analyze your lung
capacity.
Surgical Procedure
The potential benefits of transplantation cannot result from surgery alone and are
dependent upon your following the rigorous treatment plan prescribed by your
physicians. You must be aware of the potential risks and complications
outlined in this
document that can result in serious injury, and death. Your physicians
cannot predict
exactly how your body will respond to a transplant. It is never fully known how the
condition that caused your underlying kidney and/or pancreas disease will
affect your
transplant. The operation is complex and the risks are high. The overall
success rate,
roughly defined as the patient surviving with the transplanted organ for
at least one
year, is about 96‐97%%. In other words, the chance of dying following a
kidney and/or
pancreas transplant is about 3‐4% in the first year. The success rate varies
according to
how sick the patient is prior to the transplant surgery, with sicker patients having a
lower chance of a successful outcome.
Donated organs are allocated according to the policy of United Network for Organ
Sharing (UNOS). The Kidney Allocation System was revised in December 2014 and uses
a point system to calculate longevity of the kidney and the compatibility
of the donor
organ with the recipient. This system will be discussed with you by the
transplant
coordinator. Being placed on the transplant waiting list does not guarantee the
availability of a kidney and/or pancreas or receiving a transplant.
The Transplant Operation
When a donor organ becomes available, you will be called and you must come to the
hospital right away. If the organ has a Kidney Donor Profile Index (KDPI)
greater than
85% our surgeon will review this with you and assist you in making your
decision. It is at
this point that the surgeon has a clear picture of the risks associated
with this particular
organ versus the risk of waiting for the next available donor and can base
the specific
recommendations on this information. You always have the option to decline an organ.
During the transplant surgery you will be put under general anesthesia,
which means
you will be given medications to put you to sleep, block pain, and paralyze
parts of your
body. You will also be placed on a machine to help you breathe. The anesthesiologist
will talk with you in more detail about the risks of anesthesia. The transplant surgeon
will make an incision in your abdomen. Through this incision a donated
kidney and/or
pancreas will be placed into your abdomen.
Drains may be put into your body to allow fluids to be removed and to help you heal.
Special mechanical boots or sleeves around your legs will be used to keep
blood flowing
through your legs to try to prevent dangerous blood clots. You will be
in the operating
room approximately 4‐6 hours.
Post‐Surgical Care and Recovery‐ need post transplant living information
After the surgery you will be taken to the intensive care unit where you
will be closely
monitored. You will be on a machine to help you breathe and you will have
many tubes
and drains in place. Intermittent pressure boots or sleeves around your
legs will be used
to prevent blood clots.
Immediately following the surgery, you will experience pain. This will
be carefully
monitored and controlled. Most transplant recipients have a significant
reduction in the
pain two to three weeks after surgery.
When your medical condition has stabilized you will be transferred to the
transplant
floor. Your length of stay in the hospital will depend on the rate of your
recovery. You
will remain in the hospital as long as your physicians feel hospitalization
is necessary.
Most patients stay in the hospital for approximately one week, but hospitalization time
can vary depending on the severity of your illness prior to transplant
or complications
after surgery.
After you leave the hospital you will still be recovering. HERE For the
first 4‐6 weeks you
will have some restrictions on your daily activities. If you experience
any post‐operative
complications your recovery time may be longer. During the recovery period the
transplant team will follow your progress. You will need to be monitored
on a long‐term
basis and you must make yourself available for examinations, laboratory
tests and scans
of your abdomen to see how well your transplanted organ is working. Biopsies may be
done as needed to diagnose possible complications including rejection or recurrent
disease.
The transplant team will see you regularly for three to six months post
transplant. Every
effort is made to transition your routine medical care to your primary
care physician. You will be followed in the transplant clinic for life.
For most patients this involves frequent lab work and a yearly clinic
visit. Patients who develop complications may
need to be seen more often by the transplant team.
Alternative Treatments
Alternative treatments or therapies may be available for your medical condition,
including initiating or remaining on dialysis and continuing current treatment regimens
for your diabetes. Additional alternatives will be discussed with you by
the Transplant
Nephrologist.
Potential Medical/Psychosocial Risks
There are inherent risks in all surgeries, especially surgeries conducted
under general
anesthesia. Many complications are minor and get better on their own. In
some cases,
the complications are serious enough to require another surgery or medical
procedure.
Bleeding during or after surgery may require blood transfusions or blood
products that
can contain bacteria and viruses that can cause infection. Although rare, these
infections include, but are not limited to, the Human Immunodeficiency
Virus (HIV),
Hepatitis B Virus (HBV), and Hepatitis C Virus (HCV).
There may be a delay in the function of your transplanted organ. Such a delay may
increase the length of your hospital stay and increase the risk of other
complications.
There is a possibility that the transplanted organ will not function. When
this occurs a
second transplant is needed.
There are other risks associated with transplants. Infections from bacteria,
viruses, or
fungi, acute rejection, and side‐effects from drugs that suppress the immune
system are
all possible complications. Side‐effects from immune‐suppressing drugs
include kidney
problems, gastrointestinal complaints, blood count abnormalities, nerve
damage, high
blood pressure, weight gain, diabetes, and others. There may be a need
for repeated
biopsies, surgeries, and other procedures, or a prolonged intensive care
unit or hospital
stay after a transplant.
There is a slight increase in the risk of certain kinds of cancer (including
skin cancer and
post‐transplant lymphoproliferative diseases or lymphoma) because of the
immunitysuppressing
medications.
Emotional and psychosocial issues before and after transplant vary. Anxiety,
stress, and
depression have been noted. Should you experience these, please notify your
Transplant Surgeon, Transplant Nephrologist, Transplant Coordinator, or
Transplant
Social Worker.
Miscellaneous risks:
Despite the use of compression boots, blood clots may occasionally develop
in the legs and can break free and occasionally move through the heart
to the lungs. In the lungs, they can cause serious interference with breathing,
which can lead to death. Blood clots are treated with blood‐thinning drugs
that may need to be taken for an extended period of time.
The risk of infection is higher for transplant recipients than other surgical patients
because the treatments needed to prevent organ rejection make the body
less capable
of fighting infection. The abdominal incision for the transplant and any
incision needed
for the kidney bypass machine (neck, underarm, and groin) are potential sites for
infection. Infections in the sites where tubes are placed in your body
(tubes to help you
breathe, tubes in your veins to provide fluids, nutrition and to monitor
important body
functions) can cause pneumonia, blood infections and local infections.
Damage to nerves may occur. This can happen from direct contact within
the abdomen
or from pressure or positioning of the arms, lets or back during the surgery. Nerve
damage can cause numbness, weakness, paralysis and/or pain. In most cases these
symptoms are temporary, but in rare cases they can last for extended periods or even
become permanent.
Other possible complications include: injury to structures in the abdomen, pressure
sores on the skin due to positioning, burns caused by the use of electrical equipment
during surgery, damage to arteries and veins, pneumonia, heart attack,
stroke, and
permanent scarring at the site of the abdominal incision.
National and Transplant Center‐Specific Outcomes
The most current data available from the Scientific Registry of Transplant
Recipients
(SRTR) describing patient and graft survival one year after transplant
is represented in
the attached document and do not significantly differ compared to national data.
Notification of Medicare Outcome Requirements not Being Met by Center
Specific outcome requirements need to be met by transplant centers and we are
required to notify you if we do not meet those requirements. Currently, Methodist
Dallas Medical Center meets all requirements for transplant centers.
Organ Donor Risk Factors
Certain conditions in the donor may affect the success of your transplant
such as the
donor’s history and the condition of the organ when it is received
in the operating room
for your surgery. Additionally, there is a potential risk that you may
contract HIV and
other infectious diseases if they cannot be detected in the donor.
Right to Refuse Transplant
You have the choice not to undergo transplantation. If you choose not to have a
transplant, treatment for your kidney and/or pancreas disease will continue. If you do
not undergo the transplant surgery, your condition is likely to worsen.
If you have
kidney disease, dialysis will need to be initiated or continued with a
decrease in your life
expectancy.
Transplantation by a Transplant Center Not Approved by Medicare
If you have your transplant at a facility that is not approved by Medicare for
transplantation, your ability to have your immunosuppressive drugs paid for under
Medicare Part B could be affected.
After you have a transplant, health insurance companies may consider you to have a
pre‐existing condition and refuse payment for medical care, treatments
or procedures.
After the surgery, your health insurance and life insurance premiums may
increase and
remain higher. In the future, insurance companies could refuse to insure you.
Waiting Time Transfer and Multiple Listing
If listed for transplant, you have the option of being listed for transplant
at multiple
transplant centers and the ability to transfer your waiting time to a different
transplant
center without loss of the accrued waiting time.
Concerns or Grievances
The United Network for Organ Sharing provides a toll‐free patient services
line to help
transplant candidates, recipients, living donors, and family members understand organ
allocation practices and transplantation data. You may also call this number
to discuss a
problem you may be experiencing with your transplant center or the transplantation
system in general. The toll‐free patient services line number is
1‐888‐894‐6361.
Consent revision 6/17/16